“Are you going to be a specialist? Or just a GP?”
As a medical student and junior doctor in my hospital training years, I was often asked this question by friends, senior doctors and well meaning patients. It really grated on me, that one little word: “just”.
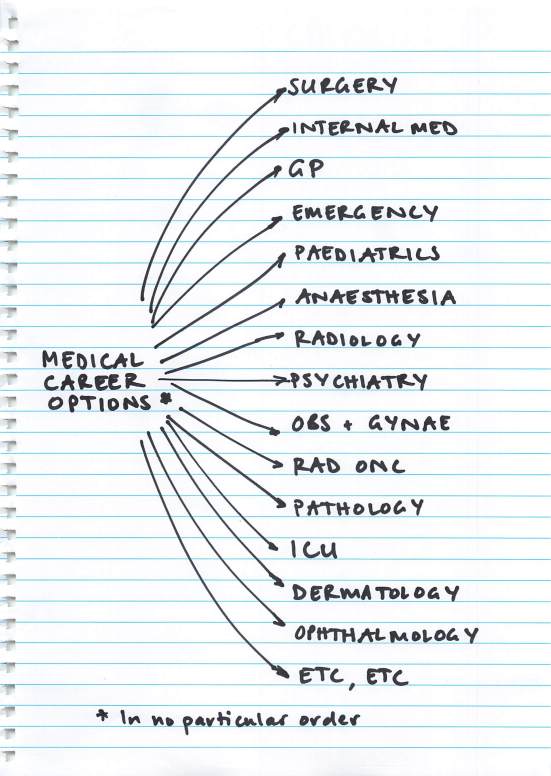
I always thought I’d become a GP. As a teenager, I was inspired to study medicine by my own GP who had always looked after my family with such care and compassion. As I went through my training I dabbled with the idea of other specialties; I was fascinating by the life stories of my geriatric patients, I loved the cute-factor of paediatrics, I was hooked on the emotional highs and lows of obstetrics, I enjoyed the team atmosphere of the emergency department. But I think, deep down, that I always knew I liked ALL of medicine too much and that above all I wanted to make a meaningful difference to my patients’ lives. For me, GP was the obvious choice.
Nowadays, when I tell people that I’m a GP, they ask instead “So are you going to specialise in anything?” They don’t seem to understand that I HAVE already specialised. I’ve specialised in General Practice (and GP obstetrics) by doing an additional 4 years of training on top of my medical degree and internship. I am officially registered with the Australian Medical Board as a “Specialist General Practitioner”. This has been a conscious decision; I haven’t just become a GP by default.
So to be asked these sorts of questions always seems so unfair. It implies that “GP” and “specialist” are two diametrically opposed alternatives, and that GP is the lessor of the two. If you’re smart, ambitious, passionate and successful you become a specialist. If you can’t get into anything else or if you want the easy option you become a GP. It’s seen as a back-up option, not as a worthwhile career in itself.
The specialist vs “just a GP” dichotomy also perpetuates the idea that GPs are not “experts” in their own right; that GPs are the amateur doctors that do the easy bits of all the other specialties and then refer on when it gets too complicated.
I’d like to dispel that myth. GPs ARE experts. We are the expert in each and every one of our patients.
We are also the experts in:
- Preventative medicine
- Undifferentiated illness
- Chronic disease management
- Complex multi-comorbidity
- Judicious use of finite medical resources
- Coordination of the health care team
We do these things better than anyone else. In fact, studies (see here and here) have repeatedly demonstrated that an increasing number of primary care doctors results in better health outcomes overall, a higher quality of health service and at a decreased cost. Whereas an increasing number of specialists is associated with higher costs and poorer quality of care, including higher overall mortality. So, as a group, GPs do a far better job at improving health outcomes and for less cost compared to specialists.
So where do all these negative attitudes come from? Unfortunately some hospital doctors perpetuate these views. They refer to General Practice dismissively as “coughs, colds and sore holes” or (particularly for female GPs) “tears and smears”. I have heard some specialists loudly criticise GPs for not knowing everything that they know about their chosen field, apparently unable to appreciate the enormous breadth of knowledge they have in other areas.
Once I even heard my university professor talk to our class about a high achieving doctor that he had gone through med school with, saying “She had so much potential, she could have been a professor of medicine. It was such a waste that she chose a career in General Practice”.
Even though the overwhelming majority of health care happens in the primary health care sector, the lion’s share of university and junior doctor teaching is done in hospitals by specialists, so it’s hardly surprising that many of our hospital counterparts have such inaccurate views of General Practice.
Admittedly, not all GPs are great teachers, and a GP rotation spent sitting in a corner of a consulting room is not likely to leave a good impression on the student. The subtleties and intricacies of a GP consult are not well appreciated by watching (or snoozing) in the background. Perhaps, as teachers, we could be doing better.
Here’s the thing. Any doctor who thinks that General Practice is easy has clearly never tried it themselves.
The reality is that General Practice is an enormously rewarding, challenging and varied career and that no two days are ever the same. We have no idea what is going to walk through our door next and it could be anything from an infant with a fever, a pregnant lady with pre-eclampsia, an elderly patient with new onset AF, a young man suffering with crippling anxiety, a parent grieving the death of a child to a full-blown heart attack. And all of these medical conditions come with added layers of complexity from the patient’s personality factors, social circumstances, family situation, expectations, medical co-morbidities, values and beliefs.
Not only do we have to be able to initially manage every single symptom and medical condition imaginable, we have to be able to do it without a full suite of investigation tools, without easy access to allied health and other specialists and all within an allocated time slot of 10-15 minutes. What’s more we are not managing that patient just for that episode of illness (or until we can turf them to another team), rather we are caring for their overall health and well being in the short, medium and longer term.
Many of us have also chosen to pursue further training in sub-specialised areas, eg obstetrics, anaesthetics, surgery, emergency medicine, aboriginal health, dermatology, paediatrics, sexual health, addiction medicine, medical education and many more. I may be in the clinic one day, and the next be performing an emergency caesarean section, or resuscitating a newborn. Really, the depth and breadth of work that we can pursue as GPs is unrivaled – and we are incredibly lucky in this respect.
Don’t get me wrong. I have a huge appreciation for my specialist (? partialist) colleagues. In particular I am grateful for the depth of knowledge and skills that they have in their niche area that I could never hope to achieve. I know that they, too, want the best outcomes for our patients and that the system works best when we all work together.
However, I’d really like for people to stop asking “are you going to be a specialist, or just a GP?” and instead to enquire “What type of doctor are you going to be?”. It’s up to all of us to change the conversation and give General Practice the respect and prestige it deserves, so that medical career choices can be seen to be more like this:
There is reason for optimism. The General Practice Student Network has over 60% of medical students as members and is doing great work to be a shining light of General Practice amidst the loud voices of hospital medicine. Also, applications to Australian General Practice Training are becoming more and more competitive. This year there were over 2000 applicants for only 1200 training places and eventually this will help to change the perception of GP as an easy back-up option if Plan A doesn’t work out.
The growing online presence of passionate GPs on social media can only help to spread the word about what we believe is the best job in the world. Check out blog posts from notjustagp.com, kidocs.org and greengp.wordpress.com on what they love about General Practice. For those of us who supervise medical students, we have the perfect opportunity to share our passion with the next generation by getting them involved in not just watching, but doing. I encourage you to let them sit in the big chair, and seat yourself in the corner so you can learn something from them, too.
To my patients: I know you may never understand the intricacies of medical training, but I want you to know that out of all the career paths on offer, I chose to be your GP; to be the person that you turn to in your time of need, to see you as a whole person and not just a diseased organ, and to be the one who helps guide you to health and wellness. I hope you know that I feel truly privileged to be your doctor.
In answer to the original question, no I’m not “just” a GP. I’m a broadly-skilled, sub-specialised, expert GP, providing a damn fine health service to my patients and my community. And I absolutely love it.
I made the best result in medical school, have masters degree in Diabetes and Endocrinology, and am a fellow of Royal Australian College of General Practitioners; I am proud to be a GP; it will be funny for any one to say that I am a GP, because I am not intelligent.
Can’t believe all these negative comments about GP’s being redundant. So ridiculous! Just because there is information available for free on the Internet does not make it reliable, especially when it comes to your health! I mean, if I want I could edit a Wikpedia or webmd articles right now and it will take them a week (maybe more) to correct it. So where would you rather get your information, from a certified professional who went to school for almost a decade or an unknown person on the Internet who probably is not even a medical professional?
Simply put
Nice piece.We will help spread the story of family medicine/GP.
Great post!
Pingback: We GPDU’d. Did you? | Nomadic GP
Love your article, spot on 🙂 you basically said everything I can think of, I wish we could read it loud on speakers in the streets everywhere 😆
Total bollocks in relation to any understanding of chronic illness – it wouldn’t be chronic otherwise!