“Are you going to be a specialist? Or just a GP?”
As a medical student and junior doctor in my hospital training years, I was often asked this question by friends, senior doctors and well meaning patients. It really grated on me, that one little word: “just”.
I always thought I’d become a GP. As a teenager, I was inspired to study medicine by my own GP who had always looked after my family with such care and compassion. As I went through my training I dabbled with the idea of other specialties; I was fascinating by the life stories of my geriatric patients, I loved the cute-factor of paediatrics, I was hooked on the emotional highs and lows of obstetrics, I enjoyed the team atmosphere of the emergency department. But I think, deep down, that I always knew I liked ALL of medicine too much and that above all I wanted to make a meaningful difference to my patients’ lives. For me, GP was the obvious choice.
Nowadays, when I tell people that I’m a GP, they ask instead “So are you going to specialise in anything?” They don’t seem to understand that I HAVE already specialised. I’ve specialised in General Practice (and GP obstetrics) by doing an additional 4 years of training on top of my medical degree and internship. I am officially registered with the Australian Medical Board as a “Specialist General Practitioner”. This has been a conscious decision; I haven’t just become a GP by default.
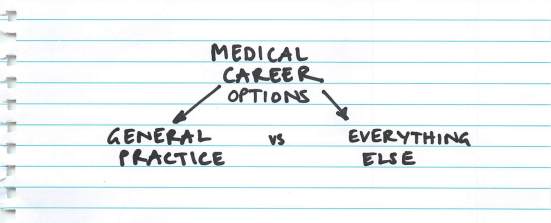
So to be asked these sorts of questions always seems so unfair. It implies that “GP” and “specialist” are two diametrically opposed alternatives, and that GP is the lessor of the two. If you’re smart, ambitious, passionate and successful you become a specialist. If you can’t get into anything else or if you want the easy option you become a GP. It’s seen as a back-up option, not as a worthwhile career in itself.
The specialist vs “just a GP” dichotomy also perpetuates the idea that GPs are not “experts” in their own right; that GPs are the amateur doctors that do the easy bits of all the other specialties and then refer on when it gets too complicated.
I’d like to dispel that myth. GPs ARE experts. We are the expert in each and every one of our patients.
We are also the experts in:
- Preventative medicine
- Undifferentiated illness
- Chronic disease management
- Complex multi-comorbidity
- Judicious use of finite medical resources
- Coordination of the health care team
We do these things better than anyone else. In fact, studies (see here and here) have repeatedly demonstrated that an increasing number of primary care doctors results in better health outcomes overall, a higher quality of health service and at a decreased cost. Whereas an increasing number of specialists is associated with higher costs and poorer quality of care, including higher overall mortality. So, as a group, GPs do a far better job at improving health outcomes and for less cost compared to specialists.
So where do all these negative attitudes come from? Unfortunately some hospital doctors perpetuate these views. They refer to General Practice dismissively as “coughs, colds and sore holes” or (particularly for female GPs) “tears and smears”. I have heard some specialists loudly criticise GPs for not knowing everything that they know about their chosen field, apparently unable to appreciate the enormous breadth of knowledge they have in other areas.
Once I even heard my university professor talk to our class about a high achieving doctor that he had gone through med school with, saying “She had so much potential, she could have been a professor of medicine. It was such a waste that she chose a career in General Practice”.
Even though the overwhelming majority of health care happens in the primary health care sector, the lion’s share of university and junior doctor teaching is done in hospitals by specialists, so it’s hardly surprising that many of our hospital counterparts have such inaccurate views of General Practice.
Admittedly, not all GPs are great teachers, and a GP rotation spent sitting in a corner of a consulting room is not likely to leave a good impression on the student. The subtleties and intricacies of a GP consult are not well appreciated by watching (or snoozing) in the background. Perhaps, as teachers, we could be doing better.
Here’s the thing. Any doctor who thinks that General Practice is easy has clearly never tried it themselves.
The reality is that General Practice is an enormously rewarding, challenging and varied career and that no two days are ever the same. We have no idea what is going to walk through our door next and it could be anything from an infant with a fever, a pregnant lady with pre-eclampsia, an elderly patient with new onset AF, a young man suffering with crippling anxiety, a parent grieving the death of a child to a full-blown heart attack. And all of these medical conditions come with added layers of complexity from the patient’s personality factors, social circumstances, family situation, expectations, medical co-morbidities, values and beliefs.
Not only do we have to be able to initially manage every single symptom and medical condition imaginable, we have to be able to do it without a full suite of investigation tools, without easy access to allied health and other specialists and all within an allocated time slot of 10-15 minutes. What’s more we are not managing that patient just for that episode of illness (or until we can turf them to another team), rather we are caring for their overall health and well being in the short, medium and longer term.
Many of us have also chosen to pursue further training in sub-specialised areas, eg obstetrics, anaesthetics, surgery, emergency medicine, aboriginal health, dermatology, paediatrics, sexual health, addiction medicine, medical education and many more. I may be in the clinic one day, and the next be performing an emergency caesarean section, or resuscitating a newborn. Really, the depth and breadth of work that we can pursue as GPs is unrivaled – and we are incredibly lucky in this respect.
Don’t get me wrong. I have a huge appreciation for my specialist (? partialist) colleagues. In particular I am grateful for the depth of knowledge and skills that they have in their niche area that I could never hope to achieve. I know that they, too, want the best outcomes for our patients and that the system works best when we all work together.
However, I’d really like for people to stop asking “are you going to be a specialist, or just a GP?” and instead to enquire “What type of doctor are you going to be?”. It’s up to all of us to change the conversation and give General Practice the respect and prestige it deserves, so that medical career choices can be seen to be more like this:
There is reason for optimism. The General Practice Student Network has over 60% of medical students as members and is doing great work to be a shining light of General Practice amidst the loud voices of hospital medicine. Also, applications to Australian General Practice Training are becoming more and more competitive. This year there were over 2000 applicants for only 1200 training places and eventually this will help to change the perception of GP as an easy back-up option if Plan A doesn’t work out.
The growing online presence of passionate GPs on social media can only help to spread the word about what we believe is the best job in the world. Check out blog posts from notjustagp.com, kidocs.org and greengp.wordpress.com on what they love about General Practice. For those of us who supervise medical students, we have the perfect opportunity to share our passion with the next generation by getting them involved in not just watching, but doing. I encourage you to let them sit in the big chair, and seat yourself in the corner so you can learn something from them, too.
To my patients: I know you may never understand the intricacies of medical training, but I want you to know that out of all the career paths on offer, I chose to be your GP; to be the person that you turn to in your time of need, to see you as a whole person and not just a diseased organ, and to be the one who helps guide you to health and wellness. I hope you know that I feel truly privileged to be your doctor.
In answer to the original question, no I’m not “just” a GP. I’m a broadly-skilled, sub-specialised, expert GP, providing a damn fine health service to my patients and my community. And I absolutely love it.

Well said. I am about to sit the exams for my FACRRM. If GP, or rural generalist, was a fallback, they wouldn’t have a 26% pass rate. The benchmark is extremely high, and so it should be. I am finding it much harder than the DRANZCOG advanced. Wish us luck for Oct 12…
Good luck!
Good luck!
Nicely written, and i feel your pain as well one of my mates father is a GP but my school mates mock GP as people who couldn’t hack specialising in a field and earn practically nothing compared to specialists. Hopefully the day when people appreciate GPs is near.
It is not helpful that people “mock” GPs but just in the same way as dealing with bullies, acceptance is the key. Sometimes what u resist will persist. We just concentrate on doing a good job…..
Loved it
Very well-written. I’m a psychiatrist and often see patients with thick files of reports from every conceivable specialist, their final stop being a neurologist or neurosurgeon (can you believe it!), which is how I get the reference. When I ask them “Who’s your GP?” the answer is “Well, we only go to specialists”. Then I proceed to tell them how important it is to have a GP who will care for all aspects of their health and refer them to a specialist if he thinks it’s necessary, while they look at me disbelievingly. Now I’ve found a way. I ask them who is a good doctor near their home, the one they go to for fever or headache, and get a history of how well he treated them when a family member was sick…you get the picture, right? It’s kind of working.
Great blog, you managed to really engage me on a subject I previously had no interest in/ knowledge of. I had a wonderful family GP growing up in a rural town. He was killed a few years ago in an accident and his death left a huge hole in the community.
General practitioners are not specialist and it is definitely not a specialisation. I have to agree with your professor’s point of view. To just be a GP when you have so much potential is a waste because a jack of all trade is a master of none. It is best to be a master at something rather than a master of nothing.
And to say that specialists give poorer quality of care and there is a higher overall mortality – this statement is definitely uncalled for and you are just undermining them and their hard work. It is a bias view since I know for a fact that specialists and GPs treat patients with very different cases. Specialists deals with cases that are more specific, critical, challenging and serious – higher mortality rate is expected. For example, a cardiac surgeon would have more challenging cases compared to a GP. Mortality risks of a patient who is being operated on would definitely be high. Because of this, I wouldn’t lump GPs and specialists under the same category.
Having said that, I do respect your decision about choosing to become a GP because you have a strong reasoning behind it. Great justification, I must say. In my country, we have a surplus of GP and most of my friends became GPs for all the wrong reasons! They are lazy to specialise and they just want to have a career in medicine because of the honor and pride of having a ‘Dr’. in front of your name. Some became doctors because their parents told them to. It is good to see a passionate doctor as you are – good luck in your future endeavours.
full disclosure – my grandfather and my uncle are both GPs. I have nothing against GP. I just do not like the idea of lumping the specialists and the GPs together because they are different.
Hang on, Ren. I’m not in the medical field ( except as a sometime patient) but even I know – medical students study the specialist areas in general at first, then take on their chosen speciality.
General Practitioners (God, bless them) carry on after completing those studies to learn more in each area. They’ve qualified as a GP long after their specialist colleagues are out there earning big bucks – and I’ve been a patient to a few specialists for whom the big bucks had been their only reason for specializing.
I’ve had two GPs who have actually solved diagnosis which had been missed by specialists – once, an oncologist, once a neurologist.
Don’t you dare undermine the value of a GP’s services, knowledge, or training. Specialists have, in my opinion, opted for a quick, short training. GPs have opted for expanding their understanding of the whole patient.
Thanks for the comment, Lynne, and for your support of GPs.
In defense of my hospital specialists colleagues though – they generally do have very long and onerous training pathways. GPs (at least in Australia) do tend to have a shorter training pathway. This is not because GP is easier, but rather because it would be impossible to ever teach the entirety of GP even if the training program was 20 years long! Both GPs and other specialists have a professional obligation to maintain their skills after qualification via ongoing professional development. But your point about GPs needing to understand the whole patient is very true. It seems like there is always more and more information we have to learn in order to continue to provide the best care for our patients, and keeping up with rapidly changing medical knowledge is quite a challenge!
Best wishes.
Hi Ren,
Your attitude is exactly the kind of misinformed view that I am trying to combat in my post.
Let me ask you how you define “specialist”.
If it is someone that has extra training and qualifications compared to a graduate doctor, than yes, we ARE specialists. We have 3-4 years of post-graduate training.
If it is someone who has particular skills and expertise that other doctors don’t have then we ARE specialists for that reason too – As outlined in the post, we have considerable expertise in chronic disease management, coordination of care, preventative medicine etc.
If it someone who deals with one type of illness or one part of the body – then no we are not specialists, we are generalists. But, by that logic, neither are other “generalists” like emergency doctors, general (internal) physicians or general paediatricians. But I bet you consider them to be specialists.
With regards to the quality of care and mortality provided by hospital / tertiary specialists vs GPs – I’m sorry you don’t agree with that argument but I didn’t make it up – you can click on the links and read the research for yourself!
You perhaps misunderstood the point: I’m not making a comparison between a single GP vs a single specialist treating a single patient with a particular condition. But, if you had one population that was served by 80% specialists and 20% GPs and another identical population that was served by 20% specialists and 80% GPs, the population with the most GPs would have better health outcomes. This concept has been demonstrated in scientific literature.
We may not be able to insert the coronary stent into the man’s arteries to safe his life during a heart attack, but if we provide good primary and preventive care and stop him from smoking and encourage him to have a healthier diet and exercise – we can prevent him from having the heart attack in the first place (and at the same time reduce his risk of diabetes, osteoarthritis, COPD, depression, stroke etc etc AND improve his quality of life).
As an aside – this excellent TED talk from David Newman shows that dietary intervention actually saves more lives from heart attack than any cardiology intervention.
Finally – I am sorry that the situation is different in your country. Out of interest, where are you from? It is a great tragedy indeed if people are deciding to pursue medicine for reasons of pride and then become lazy GPs. To me – pride is in doing the absolute best at whatever you chose to do.
Penny
PS – I would be interested in hearing your uncle’s and grandfather’s views!
Your diplomatic reaction to Ren’s comment is very impressive! And thanks for the post, too….some medical students who come across it can dare to be GPs, without having to worry about what the society thinks of GPs.
Thanks Dr Penny. Totally agree with you.
To Lynne R McAnulty-Street – when you enter the medical field people might actually listen to your views. The fact that someone has to create a blog to justify their own existence and improve their self-esteem, and the position of their peers, is simply sad. GP’s are what they are, deal with it. How many specialists write such sob stories. None. Never too late to change fields mate. I wanted to become a GP and someone woke me up by stating that 20 years down the track you will still have the same mediocre job and will always think “what if I did such and such..”.. Tell the truth buddy. Good luck
Hi Paul,
Can I ask what specialty you ended up pursuing?
Penny I would suggest Paul is either in a field where he does not need people skills (e.g. an Anaesthetist) or in one where he does not care about the lack of such skills (e.g. a Surgical discipline). Odd that someone who is so highly critical about the “need” for someone to create a blog actually spends time reading and commenting on it
Appreciate where you are coming from but let’s keep the conversation respectful. I have many wonderful anaesthetic and surgical colleagues as I’m sure you do, too.
Sorry guys, totally agree with Paul. I tried GP for a while and was totally frustrated by only ever being able to skim over areas of interest. And all the government red tape and where politicians keep moving the goal posts. Unfortunately I know a lot of ex GPs who made the switch to specialty medicine. And many who would not do it again. Sorry for sounding negative, but it’s my honest opinion. But good on you for being passionate
Hi Stephanie.
It takes all sorts of doctors to make a great health-care system and not all people will suit all specialties. For people like yourself who want to do certain things in great depth – then being a specialist is great. For people like me and Thinus and others we like to do a bit of everything and would get pretty bored doing the same narrow thing all the time. It’s not because GP is a lesser career, it’s just that is suits different personalities. In fact, in contrast to your experience, I know of many doctors who have left a career in specialisation to general practice because they realised that that was the more holistic and comprehensive type of medicine they really wanted to pursue.
Good luck with your career and I’m glad that we have dedicated specialists like yourself who can help our patients in a different way.
Stephanie as in most things in life there is more than one way of looking at what you said – I would respectfully suggest that these GPs made a switch to a Partialist role because they were unable to cope with the demands of being a GP.
It was simply easier to become a Partialist (even though that meant more studying). It takes a certain type of personality that can deal with the uncertainty of not sending every punter to a Specialist or for a bevy of tests and to know when you DO have to send a person further. Being a good GP, as opposed to being a Referologist (a species of Doctor that really messes up this argument for those of us that put effort into being good GPs) takes a lot of guts, perseverance, hours, studying and clinical skills. Some GPs are simply not able to cope with this and then become Specialists instead – and oftne they would use excuses of GP work being boring or frustrating. I would suggest just doing colonoscopies or skin exams would be an extremely boring and frustrating daily routine and would prefer the challenge of each patient being a surprise
An interesting take. In the US we see a shortage of GP’s because of the money which comes with specializing. This seems to distort our system and cause it to be way more expensive than it needs to be. Most specialists i deal with in profession as a PT immediately go to the more expensive tests and procedures which can be a quick, but short term fix, frequently not looking at the whole patient. For example i just helped a patient who went to a well regarded orthopedic knee specialist who was recommending tibial osteotomy a major life altering surgery for knee pain. But with a quick evaluation we saw that his ankle wasnt moving and his hip was week. With a couple weeks of treatment and exercise his knee pain reduced significantly. When i asked if his doctor had looked at either of these the patient said no. Specialists are invaluable of course, but someone overseeing the whole person is important and getting lost in our system tot he detriment of it.
I have just retired from practising medicine for 40 years. After 3 attempts to find a specialty that turned me on, I did GP for 15 years. I enjoyed it and I think I was quite good at it, but as I worked I realised how much psychiatry was in GP, and realised I had found my niche. By accident. I sold my practice and moved towards working 100% in mental health centres, then I worked in a tertiary referral hospital for seven years, in the last six of which I was basically an independent consultant, with my own ward. The patients on this ward would never actually see a ‘certified’ psychiatrist, just me.
Then I was seduced by a rural centre, still a referral hospital, and worked there for another seven years. I was a full member of the Department of Psychiatry, took call in the ER, had an outpatient practice, and looked after twenty patients on the psych floor. Still without any kind of specialist qualification. I do know that I did a good job. My colleagues, who were real psychiatrists would regularly consult me on matters relating to refractory psychosis, in which I had some useful experience from my work in the tertiary centre.
The point I’m trying to make is that by the time I realised I loved psychiatry, it was too late in practical terms, to embark on a residency. So I just did it.
When I was in medical school or in the early years of my career, I would never have guessed that psychiatry was my ‘bag’.
I learned a few things. First, I learned to respect GPs, I had walked in their shoes. Some of them have an awesome grasp of the entire range of medicine. I found that while most of my specialist colleagues also respected GPs, there were a few who felt that just because a doctor may not know all the ins and outs of their field, the GPs were a lesser breed, ‘half-baked’ so to speak. Just a GP!
The truth is, it takes a higher degree of skill and knowledge to be a good GP than it is to be any kind of specialist. A GP needs a whole roomful of textbooks, a specialist, even a psychiatrist, needs only about a foot of bookshelf!
I also noted something that alarmed me: In Canada, many medical schools today require that a student choose his specialty in SECOND YEAR! This is far too early, and encourages the young doctor to think in compartments. I have met a few specialists who went straight through med school into a residency for some sub-specialty, and ended up with no clue how to safely deescalate an ER crisis, or interact compassionately with a family in crisis.
Strangely, the psychiatrist colleagues I admired most were those who had come up through the ranks, as it were, and had done a year or two of GP before specialising.
Ren, the next time you see a specialist, ask him or her if he has spent any time in the forward trenches of General Practice. If he is good, he will be able to say yes.
Wow, what a great comment. It sounds like you have made an amazing contribution during your interesting and varied career. Thanks for all of your good work!
Hi Ren. I respect your opinion and your contribution to this blog. And at the same time may I challenge u with a new thought or concept. We GPs are the master of “The bigger picture”. Specialists are the master of the “Details”. We r the yin and the yang. We cannot thrive without one another.
You have defined exactly why you would never pass a GP exam, your empathy and communication skills are horrific. Perhaps you are intelligent, but then again even monkies can be trained to do the same thing over and over. You really are all that is wrong with the medical world. old fashioned stuffy, arrogant thoughts that hide a fear that you just arent good enough. Define yourself by more that your job, your title as they mean very little in the grand scheme. Measure your status by how kind, caring and compassionate you are. I feel so sorry for you.
My passion has always been practising Medicine and aiming to do that at the highest level so I covered both angles with being registered as a Gp and a Specialist Physician. This overcame minimising my opinion as a Gp by both the wider community and our colleagues allowing me to pursue our Art somewhat unfettered. However Policy Makers and Politicians are just now recognising that generalist funding is better value than specialist funding to achieve the higher good and sustain it over time and there can be NO doubt that the reservoir of good clinical medicine and critical thinking that resides in our rural Gp’s is going to be a major pool of excellence for us all to draw on.
I reckon the first Google University Professor of Medicine will be a Gp when they eventually begin the Global Medical Degree.
cheers
GP AUD$105000-120000 Everyone else AUD$275000-425000
Wow just stop giving a crap how other people see you. Problem solved.
Luckily I’m comfortable enough in myself that my sense of self-worth is not affected by other peoples attitudes. The problem is when those attitudes bias medical students and junior doctors away from considering GP training, and also potentially affect the relationship and communication between hospital doctors and GPs which is no good for the patient.
good point an good luck making a difference 🙂
Lol. May I suggest an alternative way of putting it. “Acceptance”
may I suggest you read how to win friends and influence people!
Dr Vin, if you read this post carefully, you will realize this is not a bitter rant. It’s there to create AWARENESS. People simply aren’t aware of what a GP does and what they’re good at, as such they fail to benefit from their expertise. Please ~ I am sure this blog owner is not looking for Deepak Chopra.
Hi Ann. Was referring to Vegetarianvirginrunner comment and not the post. 😊
Feeds also into health economics. The skills of GP is, frankly, sorting the wheat from the chaff. We are gatekeepers, sieving serious illness from the trivial. I might see a several hundred non specific viral infections every year…but need to be able to pick out the meningitis amongst them.
Most of my colleagues who practice single organ medicine are terrified of undifferentiated illness…as they recognise the danger and inhernt skill needed to do it well
So, a properly trained primary care physician is an asset, sorting the serious from the not so serious. To the single organ physician, every nail needs a hammer….how many times have we seen patients admitted with ‘chest pain for investigation’ under cardiology, discharged later with a ‘non cardiac’ diagnosis – but failing to identify their pneumonia, PE, gallstone etc.
Sure, in some countries unfettered doctors ar allowed to practice as GPs…those countries tend to need every Pap smear done by a gynae, every cough seen by a resp physician, every chest pain seen by a cardiologist. Health costs spiral.
An effective primary care system is worth its weight in gold. This needs skilled physicians who are specialists in primary care. They are specialists, just not in single organs!
End of.
Reblogged this on The joys and terrors of being awfully nice and commented:
Often I am asked whether I will specialize or become a GP. It is a very common misunderstanding that GPs have not specialized, perhaps a new title is in order! GSs- generalized specialists.
Exactly my thought; there may be need to adopt “Family Physicians”, which is what GPs are.
Pingback: “Are you going to be a specialist? Or just a GP?” | Write Upi..!!!
I don’t think changing the name will change the public perception. The vast majority of the public think people graduate medical school and are then automatically a GP. It’s not because of the name, it’s simply because a GP is their first point of call. A GP is what people associate with a doctor. If you are “going to see the doctor”, it means you are going to see the GP- the two words are essentially interchangeable in the public mind- which i don’t think is something that should be changed.
The idea of the us v’s them concept is not unique to GP v’s Specialist. From what i can gather in medicine, any specialty that receives referrals from another specialty, looks down at the specialty making the referrals. As somebody that works in the ED, i know that the ED probably looks down on GP land more than any other specialty, simply because we receive referrals from them (even though really the referrals are mainly for the inpatient teams, and they simply come to us because they have to).
I suspect the ED point of view is a reflection of the combination of the ED mainly seeing referrals from the 1% of crap GPs out there who send crap into the ED (and of course the other 99% who actually manage patients well and keep them out of hospital are forgotten- out of sight, out of mind), and the competitive nature of the people doing medicine- whereby getting a referral is almost seen as a “you can’t deal with this, therefore you refer it to me, therefore i am better than you”. The same then flows on. The inpatient teams all look down on the ED, likely because they see the crap inappropriate referrals from the 1% of crap ED doctors and remain oblivious to the 99% of good ED doctors who have either managed the patient or referred them to the appropriate specialty, plus also the general competitive “you can’t deal with this, therefore you refer it to me, therefore i am better than you” mentality. The same then applies to specialties referring to other specialties or sub-specialties etc etc- only this happens so much less frequently, it’s less likely to lead to a negative perception of the entire referring specialty.
And so in my mind the reasons the GPs cop the worst of it, is simply because the 1% of crap GPs making crap referrals works out to be a larger number of referrals than the 1% of crap ED doctors, which is a greater number than the 1% of general med physicians etc etc. Plus, as GPs make the most referrals, and most specialties probably get the majority of their outpatient referrals from GPs- the “you can’t deal with this, therefore you refer it to me, therefore i am better than you” thought occurs more frequently when reading referrals from GPs (simply because they make more).
To change the us vs them mentality, one would need to change the Australian medical mentality of a referral being seen as an admission of inability, which is difficult but possible. However, there will always be that 1% of any specialty that is crap and makes crap referrals. Because GPs make the most referrals and always will do, there is no real way to change the fact that within any specialty the majority of crap referrals will have come from GPs. It shouldn’t be a reflection on general practice as a whole and even though most of those specialists when thinking logically would probably realise that those crap referrals are not a reflection of the 99% of good GPs, it’s still always going to cloud the subconscious
Along the general lines of this post – our Specialist Colleagues for the most part still consider us as just GPs – yesterday my wife and I sent in two patients with calls ahead and well written thorough referral letters.
One is a 190kg 30y old with several clotting risks and disorders on Clexane. She has a large epigastric hernia with a narrow neck and and trapped small bowel and fat. No flatus or bowels open – she has some sort of dummy spit with the hospital team and leaves against medical advice – back to a country town two hours away from us – the only way we know about this is an electronic discharge by the Intern that is in my intray this morning advising me to check if her bowels has opened up and to tell her to lose weight.
Second one is is a 170kg Prader Willi – 27y old but mentally a 3y old. Presents in CCF with saturation in mid 70s – was admitted for same less than a month ago and was in ICU. Also has CRF and IDDM. He gets cranky when they try and insert a cannula (as any 3y old would) so they send him away with his sats and oedema up to the groin and BSL of > 20. I know this because his dad told me this this morning
Guess Canberra’s hospitals cannot waste time in calling mere GPs about these issues
As someone planning to go into a “specialty” medical career, I have immense respect for the people who choose GP. Personally, I could never do GP because I don’t think I have what it takes to do it. That doesn’t mean that I’ll be a bad doctor in the specialty I choose. I love my choice, and I respect the choice that everyone else makes. We need GPs just as much, if not more than we need “specialists.” It is the same attitude in Canada – that GP is what you do if you don’t want to do anything else. I think it is the wrong idea and in fact, that GP is one of the most challenging “specialties” to do. Your post could not illustrate this more!
My Doctor and friend is a GP. I said “you realize at the banquet when they ask you what you specialize in and you say GP they are all going to move away from you at the table.”
His answer? “Yeah but then I tell them I’m the one who does all the referrals and they all move back.”
Reblogged this on Medical Q-Bank.
I don’t understand why we as a society, always push someone into something they don’t want to do. If said individual is successful, I see no need to push them.
Well said. Nice post!!
I lost respect for doctors as people long ago when I had no money and MS. Then other problems arose. I actually heard a neurosurgeon say out loud “that he couldn’t stand the sound of my voice”. The other one, he was more interested in what was “out there for him tonight”. Now I have some money, insurance and an Internist who is without a doubt the biggest jerk I have ever had the misfortune of meeting. He felt the need to tell me all about his “cocaine days” when he was young in the 80’s. We are both around the same age and he erroneously assumed I was as weak minded as he. What is it with doctors? What is with the God complex? Will those jerks ever get punished for the harm, very real harm they caused by not treating me and the others today that wont get treated by dentists and other “specialists” because today they have no insurance that a doctor wants. Its outright human rights abuse. How do doctors justify their violations against human rights here in the USA? Its all in secret, (not so much anymore) eventually it will surface though with computers. Just curious, you seem nice, please don’t lose that. A few people without a few bucks will never break a practice, you will always have enough financially. Watch your Office Managers they are the cruel ones.
Sorry to hear about your negative experiences. I think the situation is quite different in the USA compared to here in Australia. Our system is not perfect but we’ve got a pretty good public health system so that folks without insurance can still access essential care. All the best.
I am certain it is much better in Australia than here in USA. In USA, without money, your just another Human Rights violation. I don’t understand how we can run around the globe acting superior when in our very own backyard Human Rights violations occur daily and by the millions.
Pingback: COPD in primary care: All You Need to Know management of COPD in your practice (Class Health) Comments | COPD
Whomever says “just” GP clearly hasn’t gotten lost with a complex condition in the system. GP’s or whatever other ‘primary’ doctors someone may see serve as beacons for the chronically ill, helping navigate an utterly hopelessly confusing system of specialists and piecing together the puzzles of complex illnesses. I personally hope to be a neurology specialist and researcher, but that’s more due to my desire to perform studies. I will always have the utmost respect for any doctor who really values their patients, and takes the time to go past the ‘average’ case and try to understand the individual’s health and the situational factors which mediate it. I have come across far too many who don’t, or can’t, and they don’t serve their patients nearly as well. I believe that those who truly do are the best doctors, regardless of ‘specialty’ or anything else.
We dearly love our GP, cradle to grave, from our baby to my 89 year old mum with dementia. The best part is not only that he seems to know everything in medicine, but he knows US as a family, holistically. Specialists are overrated, if you ask me!
While I was reading your post it was as if I was hearing myself speak. I also have always wanted to become a specialized GP and I am currently one year away from achieving that goal. But I am just tired of explaining and justifying my choice to everybody. I am from Croatia and I thought the perception of GPs was different elsewhere, but I guess it is the same everywhere. And that is just sad. While I was working in a hospital as a part of my training i heard a lot of comments like: how come you know so much, it is such a waste you chose to become a GP. Those comments made me angry because they implied a GP was less of a doctor. The truth is, you can find bad doctors in every field, and a truly bad doctor is the one who does not care and does not stand up for his patients. Instead of fighting among ourselves we should work together for the benefit of our patients and the improvement of the health system. Greetings from Zagreb
Thanks for the comment. I would love to visit Croatia one day. All the best in your career. I’m sure you will make a great difference in your patients’ lives.
Im 3rd year out of med school, and doing a phD and planning to specialise after my phD completion. I studied in a clinical school back then as a med student where everyone looked down on the choice of being a GP, but the truth is I secretly enjoyed my gp rotation, I had an excellent GP who worked from 7am to 7pm everyday and treated every patient of his respectfully and sensitively. He also let me have my own patients on weekends when he did on-calls on weekends. In med school, if anyone wants to be a GP, they are seen as losers. So to fit into my group and due to peer pressure, of course I aspired to b a specialist, and as a top student with a few papers published, my parents and my then-boyfriend
expected me to be a specialist. So here I am, a few years down the track in the research land doing a higher degree, I dont hate what I do, but I still sometimes think I want to be a GP and I think I will be really good at it. When I talk abt this again with my now husband, he would always quickly dismiss the idea and tell me “u r so good, u should be a specialist, that’s just how ushould be! ” “anyone can be a gp right? All the overseas-trained drs become GPs and they cant do specialist training, u wanna become one of them? U r better than them.” My husband is an IT guy, and regardless how much I explain being a GP is not less of a dr and in fact a good GP is invaluable, he just doesnt seem to get it or he doesnt try to understand.. But I do care about his opinion.. Should I for once not care what my loved ones think and abandon phD, go for GP training, or should I keep going and meet everyone’s expectations of me? I think if I choose a gp, many people wil be disappointed including my parents and my husband, but I think I will be happy. But doing what I am doing now itz not like I hate it either… Sorry for my messy comment, I dunno what to do sigh…
Cathy – what a difficult dilemma! It’s never too late to change your career and plenty of people change their career direction somewhere along the way. It’s a shame if your family and loved ones don’t respect your aspirations. I guess in the end, everyone is responsible for their own happiness so only you can know what it is that will give you fulfillment in your life.
Out of interest, which country are you in? You might be able to do a short rotation in GP to try it out and see if you like it? Also keep in mind that it is possible to pursue an academic career alongside general practice. GP needs high quality research, too!
All the best with your career whichever way you decide to go.
Hey Cathy…
Just wanted to say I have been struggling with similar problems and I know it’s hard to “give up” opportunities that your hard work, skills or even just plain luck of birth has led you to. Especially if you have invested many years in a certain direction.
Is your husband going to be spending every working day in your shoes? No – he is only seeing things from an outside persepctive. He is not the one who must live with “what ifs.” Do what will make you happy. Life is too short. Your family may never understand but they won’t begrudge you the happiness that comes from being true to yourself.
Dear Cathy, It sounds like you are in a bit of a bind. On one hand, you want to follow your heart and become a GP and on the other hand, you want to do Specialty because there is a general belief that it is better. I can share with u something. When you dig deep enough, everyone’s goal is to be happy and the secret to happiness is this. One has to create a life that is congruent with one’s core values or change your core values to fit in with your life. Do you know what your core values about work are? Your answer lies in there…… Hope that helps. Dr Vin @ gpexamsupport.com.au
Very well written. I am writing from the perspective of a specialist. Itis my opinion, that all of us “evolve” in our career. In med school days, my mantra was ” never ever internal medicine” which the surgeon father of mine “could very well understand”. The internships changed the perspective a bit, anaethesia, paeds and in the end internal medicine were on it, with a feeble hope of landing in nephrology. My father still can’t figure out, what went wrong 😉 and I am happy, I never chose a surgery dependent specialisation.
This much to evolution from my personal perspective, back to the topic in general:
I think, many factors influence our decision to whatever way we choose – one’s own interest and perspective, to be or not be one’s own boss, workload (of which you become aware later on), family, life and interests, hobbies (if time is left to enjoy), commitments and your interests.
I don’t think specialists work less – we have our own stress. Howvever exchanging with my GP friends I realise, that they work on a much broader spectrum in medicine and socially than many specialists do! They have to maintain themselves “a jour” on these topics and keep up a network of support to patients working together with colleagues and paramedical staff. At times they even replace family!
One of my med school colleagues was a die hard aspirant for surgery and was so frustated with the fellow ship, the peer pressure, the pressure to have your papers publicised and pursue the career, instead of being a good doctor to your patient, that he ended up to be very good GP. I don’t want to say, that career (specialists) doctors are not good doctors, but with all pressures, it may be a good to step back ans ak yourself, if you are satisfied with the care you are giving to your patients? Are you doing justice to them? to yourself? If yes, then pursue, but be loyall to yourself – a specialist or not, as a GP or not! You are not better b/c you are specialist
I work with GPs without whose support the network for many patients would not work. In the Western hemisphere, the doctors, health care givers and teachers take up lots of supportive measures, which in other cultures the family takes care of – in whatever means, they are able to.
I never wanted a specialisation, which would make me limited to my specialisation only. I chose nephrology, which incorporates internal medicine and with our dialyiss patient etc, we ware their GPs as well, giving me part of an idea of what that means and I would go for it any time again!
I have high respect for the GP’s and their multitasking! I am woman and thus a multitasker (pun intended!), but when my friend and me get together, I do realize, that we specialists hardly realize all that hard efort, which goes into the patient support.
I totally agree. It’s not whether GP or specialty is “better”. It’s whether it’s a fit for you. You can be a great doctor as a specialist or a GP, but you must love what you are doing. The other point is that as a young doctor, you can make a choice that you discover to be a mistake for you, but in most cases, you can change your mind. The only issue is age. Do you have time to make the change worthwhile? Are you still young enough to be accepted into whatever training you need? Good luck!
This is why all junior Drs should have some form of career counselling as it is not difficult to know what is right or wrong for you. All u need to do is to work out what your core values about work, family and community are and follow that path. The problem is that most people do not know what their core values are and mistakenly making a decision based on the core values of others.
Thank you for this post! It’s true that GPs are undervalued (and often underpaid, even after specialising in Family Medicine). What the world needs is far fewer specialists in developed countries/urban settings and far more generalists in places with greater need.
Medical students start off wanting to help people in a rewarding career but by the end of their training that motivation has been beaten out of them – at which point specialising in something (anything!) seems to be the “best” thing to do.
I think the medical fraternity needs to recognise the value of a doctor who does not freak out or throw a tantrum at the prospect of seeing an unselected patient in a low resource setting…
Reblogged this on physician21.
Thank you! I have been wondering about this for a while and you have really helped me with that and and considering being a GP now
Yay! Good for you!
Some very interesting comments here……This is my take on the topic. “On one hand, there is the belief that Specialists are better than GPs and the other hand, there are arguments that being a GP is just as good as being a Specialists”
The reality is that neither beliefs are necessarily helpful in the wrong context…..
For a Doctor to be happy and optimal, he or she has to do what is congruent with their core values/personality.
If your core values re work is …
1 You need flexibility
2 You need variety and accept a level of uncertainty
3 You believe in holistic care i.e. physical as well as emotional wellbeing
4 You need good work life balance or at least the ability to have this if you choose to.
5 You love continuity of care and long term connection with your patients
Then GP might be for you.
If your core values re work is ….
1 You have to do things perfectly or don’t do it at all
2 You want to be somewhat “legendary” but do not mind the poor work life balance
3 You are obsessive in nature I do not mind focussing on a small area
4 You want to be an “expert” in something and have less tolerance for uncertainty
Then Specialty might be for you.
So in essence, a Good GP is better than a Bad Specialist and a Good Specialist is better than a bad GP. The key is to know which one you are destined to be and not what your parents, peers or society want you to be!
Sharing my views..
DrVin@gpexamsupport.com.au
Thanks so much for sharing this. It is a great summary and you make some excellent points. I have half a mind to distribute your comment to every medical student and young doctor in my acquaintance.
Thanks for you kind comment Khinky.
You’re quite right. That’s a great summary, Vin.
Thanks Penny. Hopefully it can help someone.
Except a specialist
1) is completely incompetent outside of their chosen field even for basic problems
2) typically over-investigates or over-treats simple, uncomplicated presenting problems and conditions because they are more used to complex, refractory diseases.
3) expends excessive time and resources to evaluate patients compared to generalists to the detriment of the health budget
Pingback: Be a Zero, Not a Hero - KI Doc
Found this blog a bit late and after the event, so apologies for reigniting the conflagration. I can’t accept the argument that general practice is a “Specialty”. But do think that anyone who patronises GP colleagues as “just a GP” is a dickhead.
I speak from personal experience. I did most of the GP training programme around 10 years ago, and then moved into a surgical specialty. The two are worlds apart: it is a complete fallacy to equate the GP “programme” with the rigour of any other kind of specialty training – if that is the thesis of your post.
It was possible to pass the GP fellowship exam with little or next-to-no study (i.e. 4 weeks). I did 13 exams in 4 years as a specialty trainee, all the while doing 50-60 hours per week full-time work. I studied 18-24 hours per week for 9 months (in addition to working) in order to pass my specialty fellowship; this is fairly typical.
And as a specialty trainee I received none of the federal government monetary handouts given to GP trainees as incentives to keep doing it.
General Practice is a diverse discipline, but there are very few who practice it in the traditional sense described by the blogger; I would suggest that the rural generalist is perhaps the best example. However, I suggest most GPs in an urban setting spend a significant proportion of their time as “coordinators”: shuffling patients with complex problems between specialists who can actually do something, while retaining care of the simple stuff. And to regard GP as a “Specialty” is a fiction cooked up recently by AHPRA, reflecting RACGP’s political influence more than anything else.
I do agree it is offensive and ignorant to ask someone if they are “just” a GP, because it is an extremely difficult job to do well. However, it is also an extremely easy medical job to do very poorly.
It is equally offensive to regard every specialist as a neanderthal, OCD perfectionist, wasting “precious resources” by over-investigating, and without regard for a patient’s emotional wellbeing. You won’t be a very successful specialist with any of those attributes.
Similarly the myth that specialists know nothing outside their own area of expertise. Ridiculous. @DocXology I suggest you find a new bunch of specialists to care for your patients as those with which you have experience don’t seem particularly good.
– “However, it is also an extremely easy medical job to do very poorly.”
That is true of every specialty, not just generalism. Every single doctor would be able to recite cases of very poor surgical or specialist treatment.
You use the term rigour to highlight the difference between the training programs. However I would suggest that this rigour of horrible hours and over-working usually leads to the mistakes, fatigue and break-down of communication skills so often attributed (albeit at times unfairly) to surgical trainees.
– “I suggest most GPs in an urban setting spend a significant proportion of their time as “coordinators”: shuffling patients with complex problems between specialists who can actually do something,”
Most of your argument is created from anecdotes or assumptions, neither of which contribute anything substantial. As they say, the plural of anecdote does not data make.
Doesnt really matter. Half of ALL doctors of whatever ilk are ‘below average’
Be the best you can be in your personal field. That is what matters.
Good GPs, bad GPs…good neurosurgeons, bad neurosurgeons etc
Move the bell curve to the right…
There are a lot of fallacies floating around about medicine. Ultimately though, the community pays each of us to do a job that needs doing. It’s not “just” about what you want to do or why you want to do it. In that way we are like all or most others who work for a living, we live with the balance. The degree that you marry passion and practicality is the measure of your happiness and success.
If you are naive enough to equate numbers of exams or even their difficulty with some sense of importance, then your time has passed. All around the world it is your capability for a job that wins it for you and not your credentials. I honestly do not believe there is a harder job than general practice to do well. That it is also easy to be a mediocre general practitioner does not change that fact.
Well said, Janice.
“If you are naive enough to equate numbers of exams or even their difficulty with some sense of importance”
Not what I said, actually. Just highlighting the differences.
Adding more to the discussion:
“The analysis of the interviews with the participants in the referral process identified that even though there was a clear understanding of the purpose of specialist clinics the GP/specialist clinic interface was characterised by uncertainty and a lack of ownership of the communication processes.
Specialists and GPs agreed that the specialist clinics provide an avenue for GPs to have access to expert opinion, specific investigations and/or specific procedures that the GPs themselves were unable to provide to patients in the community setting. What is not clear is what ought to be managed in the community, how conditions could be managed in the community and who should take ownership of that. As a consequence, what is deemed as appropriate referral is likely to be viewed differently by GPs, specialists and unit managers at different times.”
Click to access DH%20Report%20011010.pdf
In Ontario they changed the funding model so that GPs are paid the same as specialists. They also put specialists on salaries, not FFS, and the specialists spent some of their time working out of GP rooms. Thus the incentive was to return patients to the GP ASAP, instead of hanging on to them for routine follow up as occurs here often enough (more FFS and importantly for our economy at a higher rate than the GP). It also encouraged specialists to educate the GPs who referred to them, partly because it was an essential part of their job to do so, but also to help everyone – specialists and GPs – to work to the top of their ticket. This is how I first worked with specialists too, not that long ago. Sometimes we saw the patients together – not just in the hospital but also together in my practice. Funding and practice models we have in Australia do not encourage working collaboratively this way, nor do they incentivise working to the top of our tickets – in my view quite the opposite.
Pingback: The Accidental Writer | Nomadic GP
Great article. I found it a bit late in the discussion!
I’m a specialist in medical oncology, currently completing dual training in general medicine. It pisses me off mightily when people talk about friends or colleagues being ‘just a GP’ – and I take every opportunity to point out the years of specialist training that GPs require to enter the field.
I have a deep and abiding respect for my GP colleagues, as my past residents would no doubt report, I’m a stickler for a detailed and thorough discharge summary (and a phone call!), because we know that you do 90% of the work in managing our complex (often palliative) patients. I contemplated GP training myself in internship, but in the end physician training was a better fit – I’m too perfectionistic and detail-focused to be satisfied with a shorter consultation and more general clinical care.
That’s what people who aren’t medical probably don’t understand – there’s no us and them (or at least that’s not how I think about it, nor do most of my generation of recently qualified physicians), it’s just what fits for different people.
What I can certainly understand about my hospital specialist colleagues’ frustration is the *occasional* poor quality GP referral that (in their mind) taints the entire profession. I have personally triaged many referrals that were a complete waste of a public outpatient specialist clinic’s time, referred in by GPs (and specialists too!) who, for whatever reason, felt that they were inadequate to the task of investigating and managing their patient’s presenting complaint.
HOWEVER, what I think some senior specialists forget is there are infinitely more such cases that are NOT referred on because an experienced, compassionate and thorough GP has provided good primary care without tossing them in the ‘too hard basket’ of referral to specialist services.
In other words, there are SOME poorly trained/supported/experienced GPs (and specialists!) who make providing good, timely, cost-effective care to patients very challenging. And that can be frustrating when you’re trying to juggle the over-stretched, under-resourced demands of a public hospital specialist unit.
As a future general physician, I can also vouch for my frustration at the over-specialisation of medicine, the corridor arguments about ‘taking the patient’ and the referral-centric hospital culture that stymies good patient care and outcomes. There have been a lot of people looking at the revitalisation of acute general medicine as a clinical specialty over the last few years and I’m pretty sure all of my GP and specialist colleagues think it’s a good idea.
Thanks again for the blog 🙂
Here is a cynical take…
Some specialists aren’t too interested in providing detailed feedback or better education because it might empower GPs too much.
Much better to stay vague and ambiguous and perpetuate the mystique of knowledge.
Hi Penny,
As a GP who made a proactive choice into the specialty, this fantastically written article resonates with me.
Thoroughly enjoying your take on the world, thru your other blog articles!
Thank you for sharing your gift(s) 🙂
Not read all comments but surely a better question is ‘are you going to be a GP or just a specialist?’. Reality is that a GP needs to keep up to date with numerous fields including clinical and non clinical i.e management, politics finance etc especially here in UK.
The thought that GPs are subpar to a hospital consultant in a speciality is nothing more than archaic thinking. Primary care is one of the main reasons healthcare is improving worldwide and the only way to offer cost effective universal care to a population.
My conflict here is I am a GP and proud to be one. I teach how to be a GP and will continue to battle the tide of thinking that GPs are not equivalent to a specialist. In fact we are. GPs are specialists of generalism. I also challenge ANY specialist to match the GP method of risk management: one area that marks a true clinician’s ability to offer holistic care to a patient.
Education, communication and back Primary care.
#1careRevolution
I probably don’t need to point out that the reason GP training is now becoming so competitive is that the number of graduating medical students around Australia has more than doubled over the last 10 years without a proportionate increase in available training places in all specialities. However, relative to other training programs it is still relatively less competitive to enter (for the time being). So I would dare say that the reason why more people are applying to GP training is not because of promotional efforts by GPSN or GPs who portray it as a more attractive or prestigious specialty but because junior doctors are desperate to get into a training program of any sort given that medical unemployment is now a real possibility. Also, some GPs are extremely pessimistic about the future of the profession. I was speaking to a GP yesterday (who now works in occupational health) who essentially said that GPs won’t have jobs in 10 years time because the government is taking more and more away from them and lesser trained professionals (e.g. nurses, US style physicians assistants) can do the job for less pay. Even some GPs see themselves as deskilled, poorly remunerated, paper pushing referral machines. This is a shame, as a medical student myself I intend on going into general practice based on the all the reasons you described in your post. However, if GPs truly become redundant and replaceable in the future by lesser trained professionals I may have to find something else to do.
You make a good point about the higher competitiveness for training positions across the board, but it’s also certainly true that GP is no longer the “easy fall back” it used to be for those unsuccessful in other areas. It sounds like you’ve come across some pretty cynical, burnt out GPs to give you that gloomy view of the future of GP. Yes, there are challenges ahead, there always have been and always will be. It’s my sincere hope that governments and health bureaucrats will eventually appreciate the cost effectiveness and efficiency of the primary care sector and divert more funding away from specialist care and back in to primary care for the good of the patients and the sustainability of the entire health system. There are always opportunities for those of us up-and-coming to step up and have our voices heard to make a difference in this world. Good luck with your future endeavors.
Reblogged this on chocollatra.
As a registered nurse, I completely understand where you are coming from. Our profession suffers the same stigma, but not just general nursing, all nursing suffers this. People say “oh your just a nurse” and things similar. Or ask if we chose it because we didn’t get the marks for medicine, like nursing is a fall back poor man’s option. I have defended GP medicine so many times when talking to junior doctors at work, who wrongly think GP medicine is just a fall back second choice option. More work needs to be done to educate junior doctors on what a specialised field GP medicine is. I have great respect for my GP, he is a well qualified, highly knowledgeable doctor. I think it’s the lazy blasé GP’s out there that ruin the reputation of GP medicine. You know the ones that are only there cause they need an income, but couldn’t give a toss about the patients. We all know at least one. Both GP medicine and nursing, need work done to improve their reputations to remove the word “just” from conversations. Thanks for a great article.
Personally,I have found G.P’s to often be more personable and “human” to talk to whereas I’ve found many Specialists to be arrogant and full of self important.
Ultimately,our self worth should not be measurised by what job role we do,or how much we earn,and especially not by what others think of us or if they give us “prestige”
These are inner issues that need to be worked on-whether they stem from a fragile ego(insecurity issues) or simply reevaluating what’s important in life.
Motive for going into medicines should be passion,and to serve others selflessly & not how much money or holidays I can go on,or wanting the title “doctor” in front of my name so people will think I’m important and special etc..
I believe Specialists are overpaid & there should be a new system where they are only paid if the patient deems that they have helped them instead of “referring them on” to someone else etc.In most other Professions people only get paid once they’ve earned it,eg:hairdressers don’t get $100+ just for “consulting” about someone’s hair.
There’s is a huge gap between the rich & the poor in this Country & the lifestyle difference between doctor specialists & others (indigenous,mentally ill,carers of people with Dementia etc) is huge,so only paying according to their efforts is a good idea to help close this gap.
There’s often selfishness amongst some Specialists & they’re there for the wrong reasons.
I’d rather fund for an Indigenous families first holiday,for example,then a Specialists 10th or so Overseas holiday.
Be proud that your a G.P,commit to excellence at all you do,try not to be sensitive when people say “just a g.p” because some people just say it for “ease of words” without illmeaning but if a person does say it with the feeling/intent of suggesting your “less then” a Specialist,understand that often the issue lies with them-their own feelings of inadequacies being projecting onto you/others.
Following a good path is not always without difficulties.
I became a GP after sampling various hospital specialties and finding that General Practice was by far the most challenging and the most difficult to do well. Our specialty is humanity, often helping patients to cope for years with what is left after they have been processed by the hospital system. On the whole I have great admiration for the expertise of my hospital colleagues but don’t for one minute think that I or my GP colleagues with whom I work couldn’t have equally succeeded in any one of them. I did however realise that hospital specialisation and superspecialisation was in some cases creating ‘body technicians’ rather than physicians and ‘doctors’ in the traditional meaning of the word and I have observed some quite appalling behaviour both as a colleague and a patient from some hospital specialists for which I would instantly fail any GP trainee!
First I want to say that I have been seeing all types of doctors for roughly half my life (I’m 22) so I’m making my comments based on my experances both current and past. Every time I’ve been referred to a specialist it has been because my GP has been unable to offically make a diagnosis, isn’t sure how to proceed with treatment, and frankly doesn’t know what to do. A GP simply can’t manage such a large and complicated case, this became more apparent the sicker I got. Now my psychiatrist, neurologist, rhumy, upper GI surgon, gastroentetologist, and psychologist pretty much run my long term treatment. I currently only see my GP to refresh referals or for things like a cold simply because my case is much too complicated for her to be able to look after me properly. I consider this a good thing given the horror stories associated with GPs handing out antibiotics and psychiatric medicatons like lollies. Yes a GP should always know what is going on and they should also be your first point of call, however due to the large amount of different topics they need to know about they simply can’t effectivly manage multiple conditions in one person.
I am in the slightly unusual position of being a GP whose background involves working in a broad range of medical specialities for 5 years ,achieving the MRCP(UK) diploma, before opting with several ounces of regret for General Practice because in order to get a training position in my preferred speciality after Kallmanisation (in the UK) I was required to undertake a PhD.Call me lazy, but this did not strike me as worthwhile.
I have worked in a number of GP surgeries and I have concluded that most GPs are lacking in knowledge, devoid of any degree of diligence but keen to ensure the trite aspects of care are fulfilled (you know the ones, typically attracting renumeration such as ‘lifestyle counselling’). Simple things like reading the notes/correspondence/investigation results before calling the hapless patients in seems to be asking far too much; a patient may have uncontrolled blood pressure or deranged thyroid function or an anemia which hasn’t been thought about (or even noticed because the notes have not been adequately perused) and the issue the patient presents with on the day is the only aspect which the GP considers in their interaction with the patient. Working in such an environment I find difficult and depressing because my approach as a ‘proper’ Primary Care Physician means that I will always check the notes thoroughly despite the inevitable consequence that I will finish later than my colleagues and often with a vast amount of resentment stemming from the inescapable conclusion (in my mind) that I am clearing up behind their less than diligent approach. I aim to treat patients as I would like an ill relative of mine to be treated ie with a comprehensive use of the available information, not simply a cursory look at what went on the last time they visited.
I can also fully understand hospital specialists being dismissive of general practise because, in my experience, many GPs appear to simply ignore any requests they make such as arranging this test/input/referral/uptitration of a medications’ dose etc.
The training of GPs in this day and age makes the earning of the MRCGP diploma a vital pre-requisite to becoming an independent practitioner; I find it perverse and laughable that the clinical skills station has actors and no assessment of the hands-on clinical skills of examination is at any point made of the candidate.
So to sum up, general practise in my opinion is superficial medicine done badly and the only way I have been able to continue my role in the farce, to a standard I personally deem acceptable, is to work part-time.
Sorry to hear that that’s your experience. The great dilemma of general practice is that it’s so easy to be a bad GP, but so hard to be a good one. Good on you for your efforts to be a good one.
I think only GPs think General practice as a specialty. Even on the medicare forms, there is a box for specialist and there is a box for GPs. We can also tell by our pay and the length of our training. But who cares about whether GPs are specialist or not? As long as we are providing good care and we practice good medicine, that’s all it matters. Can’t believe I just waste my time getting into this meaningless argument.
general practitioners are fairly irrelevant these days with the information on the internet.All they do is refer you to a specialist. A lot of prescription drugs should not be prescribed by a doctor with the information on the internet. I find most of them are not as well informed about my condition as I am when I present. Also it seems they are so hit and miss. You might get some guy who was trained 30 years ago and doesn’t know the latest therapies.
GP’s are a waste of time and money. Any educated person can research their condition on the internet
Obstetricians are overrated also mostly their work can be performed by midwifes- they are also self fulfilling in trying to guide people towards caesareans
Well written article. From someone who spent years in a particular hospital specialty , I totally agree about the overall power and efficacy of preventive health than spending tons of money on very unwell patients who should have had better care initiated at an earlier stage. Specialists suffer from a narrow myopic tunnel vision and actually believe that their specialty is the be all and end all.